My experience as a nurse in the United Kingdom has deeply influenced my perspective on providing care to patients with respect and dignity. In my journey through a vibrant and varied healthcare system, I met people from all backgrounds, each carrying their own distinct needs, fears, and dreams. This experience made me realize how important it is to weave dignity into every part of care. Nurses spend more time with patients than any other healthcare professional, which places us in a unique position to advocate for dignity in care.
Embracing dignity in care goes beyond just an idea; it reflects a heartfelt promise to acknowledge and respect the humanity of every patient. This piece delves into the principles of dignity in care and their application throughout different areas of the hospital. It highlights the significance of these principles, not just for enhancing patient outcomes but also for upholding the ethical standards of nursing practice.
What Is Dignity in Care?
When we talk about dignity in care, we're focusing on delivering healthcare in a way that honors each patient's respect, independence, and individuality. It includes practices that encourage independence and allow for personal choice. It’s all about focusing on what matters most to the patient — respecting their values and preferences, protecting their privacy, and providing care that’s rooted in empathy, compassion, and fairness.
Providing care with dignity is essential; it forms the basis of trust and deepens the connection between caregiver and patient.
Applying Dignity in Care Across the Hospital Setting
1. Admission Process
The hospital admission process can be overwhelming for patients. During this critical first interaction, dignity in care can be demonstrated by:
- Respectful Communication: Introduce yourself, explain your role, and outline what the patient can expect.
- Sample statement: “Hello, my name is [Your Name], and I’ll be one of your nurses today. I’d like to explain what will happen during your admission.”
- Involving Patients: Ask questions to understand their preferences and needs: “Is there anything specific you’d like us to know about your care?”
- Privacy: Ensure conversations about medical history and personal details occur in a private setting.
2. Bedside Care
As the cornerstone of nursing practice, bedside care offers countless opportunities to uphold dignity. Key practices include:
- Listening Actively: Take time to listen to patient concerns without interruption.
- Sample statement: “I hear that you’re feeling anxious about this test. Let’s talk about any questions or worries you have.”
- Personalized Care: Tailor interventions to align with patient preferences, such as adjusting the room temperature or positioning them comfortably.
- Respecting Privacy: Use curtains or screens during examinations and procedures, always explaining what you are about to do.
- Sample statement: “I’ll close the curtain now to ensure your privacy while we change the dressing.”
- This is an example of narrating care to the patient.
3. Medication Administration
Patients may feel vulnerable during medication administration, especially if they do not fully understand their treatment plan. Uphold dignity in care by:
- Providing Clear Explanations: Explain what each medication is for and address any concerns.
- Sample statement: “This medication is to help manage your blood pressure. Do you have any questions about it?”
- Seeking Consent: Ask, “Are you ready to take your medication now?” before proceeding.
- Supporting Autonomy: Encourage patients to administer their medication if appropriate, fostering a sense of control.
4. Mealtime Assistance
Mealtime can be a deeply personal experience. While assisting patients, dignity in care involves:
- Offering Choices: Allow patients to choose their meals whenever possible.
- Sample statement: “Would you like soup or salad to start with your lunch?”
- Encouraging Independence: Provide adaptive utensils or position trays for easier access.
- Respecting Preferences: Acknowledge cultural or religious dietary needs and advocate for alternatives when necessary. Some hospitals allow patients or family members to bring home-cooked meals as long as they follow dietary restrictions.
5. End-of-Life Care
Providing dignified care at the end of life is one of the most meaningful responsibilities of a nurse. This includes:
- Creating a Peaceful Environment: Ensure the patient’s comfort by managing pain, adjusting lighting, and allowing family presence.
- Sample statement: “Would you like me to dim the lights or bring in a chair for your family member?”
- Respecting Wishes: Honor advance directives and patient preferences for care.
- Showing Compassion: Offer emotional support to both the patient and their loved ones, demonstrating empathy and understanding.
6. Discharge Planning
The discharge process is a transition that can create anxiety for patients. To maintain dignity:
- Educate Thoroughly: Provide clear, written, and verbal instructions for post-hospital care.
- Empower Decision-Making: Collaborate with the patient to create a plan that aligns with their goals and abilities.
- Sample statement: “Let’s review your discharge instructions together. What questions do you have about your recovery at home?”
- Follow Up: Encourage questions and provide contact information for additional support.
All in all, an essential framework for understanding and implementing dignity in care is reflected in the 10 Dignity Challenges (SCIE, 2009, as cited in Burgess, 2020). These challenges outline key areas where healthcare professionals can foster respect, autonomy, and compassionate care. By integrating these principles into daily practice, nurses can create an environment where patients feel valued, heard, and supported. The table below summarizes these 10 key dignity challenges:
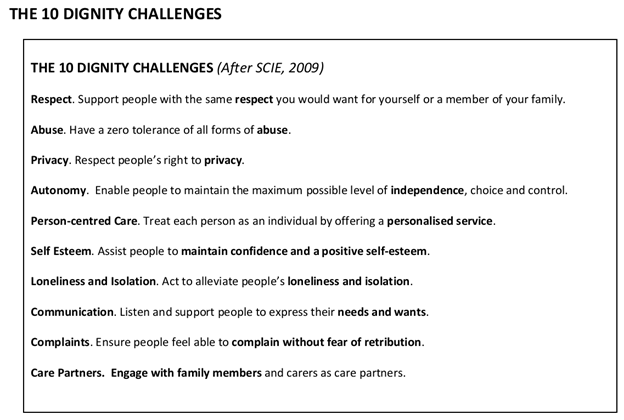
Source: Burgess (2010)
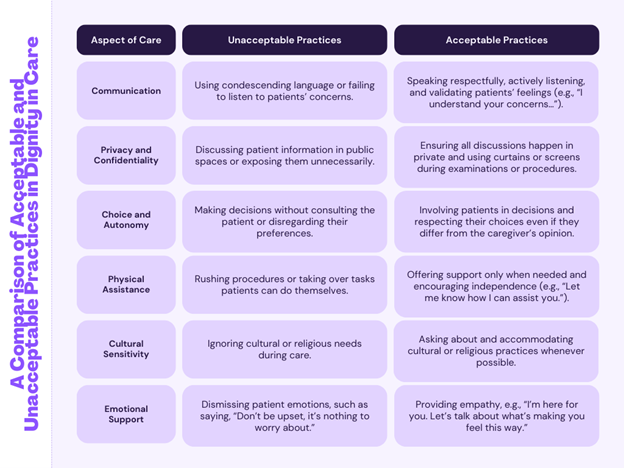
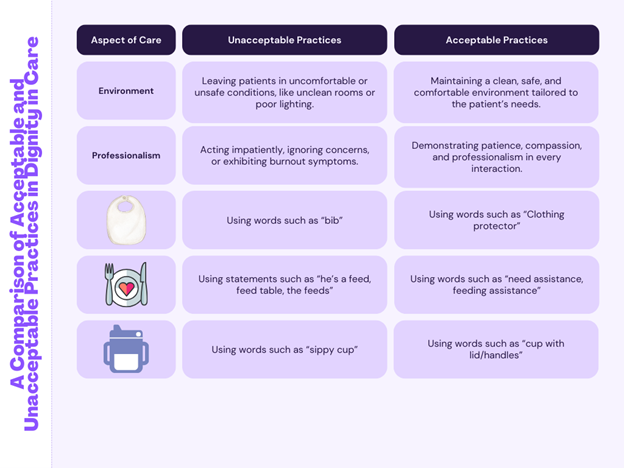
Charts provided by Blaise Nieve
Conclusion
Dignity in care is not merely an ideal — it is a tangible practice that transforms hospital interactions into meaningful experiences for both patients and providers. From admission to discharge, every point of care presents an opportunity to uphold respect, autonomy, and compassion. As nurses, let us lead the charge in making dignity a non-negotiable standard in every patient encounter.
References
Burgess, J.W. (2010). HASCAS dignity through action (vulnerable adults) resource 2: Dignity Workshop Pack. https://www.dignityincare.org.uk/_assets/Vulnerable_Adults_Dignity_Workshop_Pack.pdf
Ekpenyong, M. S., Nyashanu, M., Ossey-Nweze, C., & Serrant, L. (2021). Exploring the perceptions of dignity among patients and nurses in hospital and community settings: an integrative review. Journal of Research in Nursing, 26(6), 517–537. https://doi.org/10.1177/1744987121997890
Social Care Institute for Excellence (SCIE). (2023, September 15). Defining dignity in care - SCIE. SCIE. https://www.scie.org.uk/providing-care/dignity-in-care/defining/
Social Care Institute for Excellence (SCIE). (2023, September 15). Dignity: Information and good communication - SCIE. SCIE. https://www.scie.org.uk/providing-care/dignity-in-care/communication/
Content published on the Medical-Surgical Monitor represents the views, thoughts, and opinions of the authors and may not necessarily reflect the views, thoughts, and opinions of the Academy of Medical-Surgical Nurses.