Did you know that hospitalized patients can lose up to 10% of their muscle strength and tone in as little as one day? Hospitalized patients spend most of their hospital stay in bed. Mobility is not well emphasized considering the negative outcomes associated with immobility, such as increased length of stay and hospital-acquired harms (e.g., pressure ulcers, infections, falls).
Immobile patients are at high risk of losing functional independence, leading to increased physical demand and risk of injury for nursing and therapy staff. Barriers that exist with mobility include staffing, equipment, and processes that encourage safe patient handling. Research is clear that immobility is a direct driver for worse patient outcomes — both during hospitalization and once the patient is discharged.
A standardized assessment tool is key to understanding a patient’s current mobility capabilities and setting goals to enhance their mobility during their hospital stay. Without a tool to assess current mobility status, the ability to make a mobility goal is much more challenging. A tool allows for a starting point to better understand next steps and establish goals to address it.
Supporting the need for the implementation of a mobility tool includes:
- Type and frequency for mobility expectations. Have you ever been unsure what activities your patients should be doing? You’re not alone. Many bedside nurses feel the type and frequency of mobility is unknown with their patients. There are moments throughout the shift where movement can happen without requiring a lot of time or coordination. Mobility does not have to mean walking. It can be sitting on the side of the bed to take routine medications or standing during a bed linen change. A standard tool sets these expectations for what is needed.
- Documentation expectations of activity and mobility events. Expectations of activity and mobility documentation is unclear and often goes undocumented due to lack of clarity. By establishing task alerts and a defined practice, the expectation for charting these events becomes clearer.
- Nursing and therapy services establishing a common language around mobility. Nursing and therapy often speak differently about mobility because there isn’t a common language or tool to communicate the patient’s mobility status. Utilizing a common tool allows for better communication and a streamlined approach when discussing mobility between individuals and teams.
- Safe patient handling equipment training for nursing. Nurses who are unfamiliar with patient handling equipment were less likely to use the equipment or will possibly use it incorrectly. By providing nursing staff with equipment training, they are more likely to use it to mobilize their patients and use it correctly. It not only provides training for safe mobility of patients but also can protect staff from injury.
Mobility programs such as the Johns Hopkins — Activity and Mobility Promotion (JH-AMP) have demonstrated improvements in outcomes, such as decreased length of stay (LOS). The JH-AMP program was associated with a reduction in LOS by half a day on average. This could be due to the Activity Measure for Post-Acute Care (AM-PAC) scores being a good predictor of post-acute rehab needs so planning can begin earlier. It was also found that the tool increased the frequency and consistency of mobility.
Autonomy in patient activities also led to improvements in nursing outcomes such as decrease in turnover, burnout and injury. Common language around mobility was developed without an increase in nursing burdensome indicators measured by an increase in stress from documentation or frustration with additional tasks. Thoughtful planning and implementation of a mobility program is instrumental for success. To overcome barriers to implementation, careful planning and support are necessary. A positive culture change needs support early, with goal-directed mobility implemented by nurses.
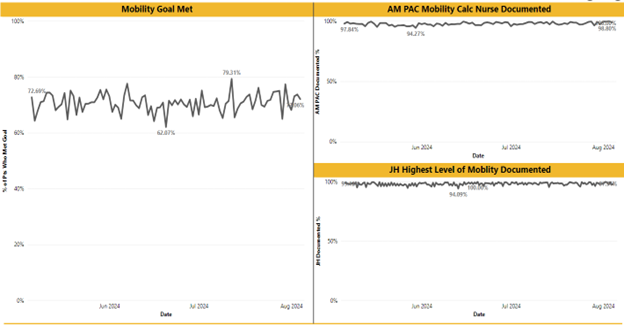
Identifying gaps in mobility practices can help with determining ways to overcome them. Figure 1 outlines primary and secondary drivers to consider in order to increase daily patient mobility goals. Highlighting these drivers can assist in developing a plan to overcome barriers. Developing a dashboard or periodically analyzing documentation to assess for fallouts is necessary for sustainability (Figure 2).
A culture of mobility is necessary to improve the care provided to patients and reduce negative outcomes associated with immobility. Implementing a standard tool for hospitalized patients requires stakeholders in various areas and buy-in with change management tactics. However, the teams involved in the patient’s care are more likely to achieve mobility goals for their patients together and see the positive outcomes associated with this change in culture.
Figure 1. Driver diagram used to determine the project aim and factors to consider when working to achieve the goal.
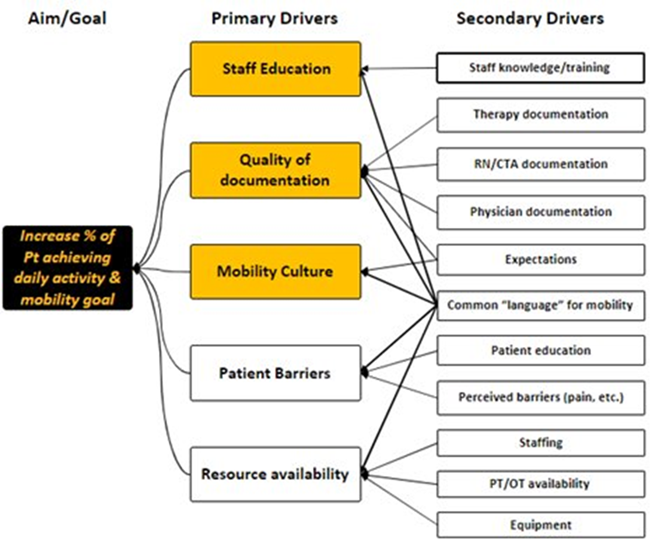
Figure 2. Percentage of daily mobility goal being met, including key wins and lessons learned.
Reference
MUHC Nursing: Process Outcomes. (2024). Microsoft 365: Power-bi
Content published on the Medical-Surgical Monitor represents the views, thoughts, and opinions of the authors and may not necessarily reflect the views, thoughts, and opinions of the Academy of Medical-Surgical Nurses.